UTMB Health’s Clear Lake Campus Hospital is one of 10 locations in the United States to launch a new heart ablation procedure that provides a host of advantages over existing techniques used to treat atrial fibrillation and other electrophysiological
issues.
The new procedure can be completed more quickly and is considered safer because it does not cause thermal damage to surrounding cells that are not being targeted.
Dr. M. Dean Sabayon, assistant professor and director of Cardiac Electrophysiology, performed the initial Pulse Field Ablation surgeries in the catheterization lab.
“This is a paradigm shift in ablation technology,” Sabayon said. “It’s really the newest, most innovative treatment modality for atrial fibrillation, and the number one advantage of this is that it is safer and more efficient—and
it basically eliminates the need for general anesthesia.”
PFA technology uses electrical pulses to kill targeted cardiac muscle cells, creating scar tissue that blocks the faulty electrical signals that cause atrial fibrillation, an irregular—often rapid—heartbeat. The 4,000 volts of electricity
used kill targeted heart cells but not other nearby cells.
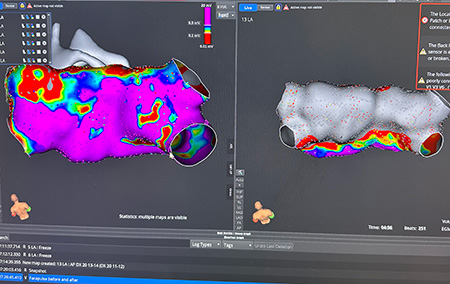
The most common types of ablation are radio frequency, which damages the target cells with heat, and cryogenic, which freezes those cells. Both techniques pose some risk of esophageal injury, phrenic nerve damage and inflammation.
Sabayon worked with an array of colleagues—from clinicians to hospital administrators—over almost three years to bring this new technology to UTMB. This included involvement in clinical trials, training on animal models and acquiring necessary
medical equipment and supplies.
Ultimately, patients should reap the benefits.
“The risk of collateral damage with this is pretty much zero, based on the studies,” Sabayon said. “In the next five years, I think everything will be moving to this.”
UTMB patients will soon have access to PFA at the Galveston campus as well.
“The working time is 20 to 30 minutes,” Sabayon said. “So, we’re able to cut back on our backlog of patients. They don’t have to wait for weeks to get scheduled. Patients come in the morning, leave in the afternoon, and there
are no restrictions or limitations. We do it with deep sedation, and so there are no risks associated with general anesthesia.”
Radio frequency and cryogenic ablations usually take an hour or more. With care teams seeing an increase in the number of patients who need ablation procedures, the capacity to treat more patients in a day is welcome. Also, some patients who were not
good candidates for ablation might be now.
“We can treat patients who are a bit more sick,” Sabayon said.